Thank you for editing your post. ![]()
How important is family history? I plan to dig through my mom’s old medical files to find more detail about her osteoporisis and treatments. But when I got a lot of detail from her years ago about her glaucoma (and her father’s), really the doctor mostly just wanted to know there was a family history - yes/no.
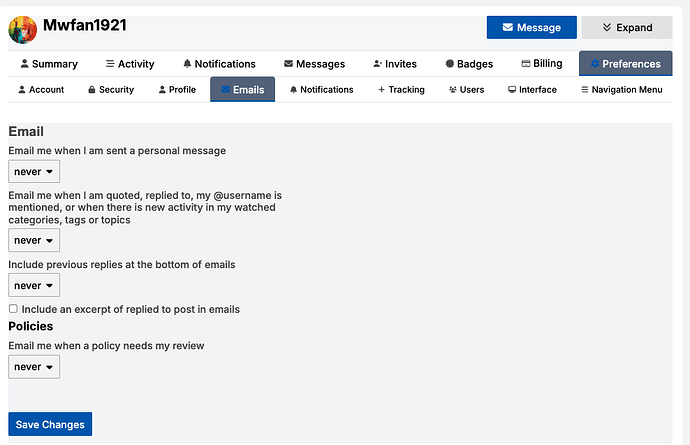
You can turn off email notifications in your account, choose ‘preferences’ then ‘email’ and you’ll see this:
I think it’s one of those things that family history could be valuable to know - family history can increase your chances of having osteo. But also since a fairly simple test can be done to diagnose it, no worries if you can’t dig anything up. And as mentioned above, our mothers or grandmothers may not have been offered up the testing - or had it available - to be tested.
Thyroid issues can also be another indicator.
My mother had Osteopetrosis. As far as I know, she did not take any medication for it. She broke several bones throughout her lifetime, including an arm fracture in her late 70s.
I am pretty sure my grandmother also had it. She was never diagnosed, never broke any bones, but lost a lot of height in her later life.
I guess I can’t really know for sure if this family history contributes to me having it.
Family history is not usually important other than that having a parent with a history of especially early or severe osteoporosis might prompt you to get an initial DEXA earlier than 65.
My own mother, in her mid 70s, does not have osteoporosis or even osteopenia. She has hated her “peasant build” all her life, but does appreciate having strong bones.
I still plan to do my initial screening DEXA at the regular time. My mother having unusually good bones doesn’t ensure I will.
This is very true. Having thyroid levels that are too high causes bone loss.
Some women with hypothyroid (low thyroid) beg their doctors to increase their Synthroid (thyroid replacement pill) beyond the normal range. They like how running high gives them extra energy and helps them lose weight. But this is terrible for your bones! Some women do it anyway; I’ve run into women who get prescriptions of thyroid from multiple doctors in order to take extra.
Omg, that’s terrible!
Family history needs to be taken into context. My mom was on meds for osteoporosis but she had decades of inhaled coticosteroid inhaler use (asthma) and was physically inactive. Neither of those two things are true for either me or my sister.
I’ve posted my story before, but I know that we have new readers. I am built much like my mom, and she had severe osteoporosis. However, there are differences in our health journey. She had breast cancer at 60 and had chemo. She took estrogen before the cancer diagnosis and tamoxifen after chemo. So her baseline health was affected by medications that I never took. She took Fosamax for quite a few years - more than what we now know is wise (without a medication vacation). While on Fosamax, she had a number of broken bones. The breaks were shear breaks, which were difficult to heal. Her final break was a thigh bone break, and it directly led to her death at age 76 (from an infection). My mom’s health history has given me pause, and I am extremely careful about how I approach medication to manage my health. I don’t eschew medication … I’ve been on synthetic thyroid since I was 16, and I know that it’s necessary to keep my thyroid levels in a healthy range. But when it comes to other meds, I am very cautious.
That is my story, though, and I respect the choices that others make about their own health. In the end, we all have to do what we think is best for us.
I take a low dosage of Lexapro (5mg per day) and I just read that SSRI’s can cause bone loss. I wonder if that has anything to do with my bone density. I’ve only been taking it for maybe 18 months so not sure if that’s considered “long term”.
My PCP ordered my first Dexa scan (age 59) a few years ago based on me mentioning my mother’s osteoporosis. Results were normal, with PCP suggestion for another in 3years adding left hip and L1-L4. I do have some summary health notes on Mom (she was quite the record keeper), and at age 64 her osteoporosis was noticed from chest xray(?). She was in a study with Fisomax 2 years, 3% improvement. Switched to weekly Actonel. Not sure how long she took that
A low dose of Lexapro for a short time (18 months is short) would not be the cause of any significant bone density problems.
Just got back from my latest DEXA scan - results were in MyChart before I got home! So first thing I did was pull my last results and next thing was skim through this thread. I had one at age 50, and I think 60, then for sure age 66, which is now considered my baseline, again at almost 71, and now just past 73.
After my previous one, my doctor advised increasing my Caltrate 600 D+ from once to twice a day (which I did last year), and consider bisphosphonate treatment (which I did not choose to do).
So my T scores: right femur went from -0.7 to -0.8, left femur unchanged at -1.3, and lumbar spine from 0.5 to 0.0.
My TBS adjusted FRAX went from: Major osteoporotic was 22.7%, now 21.2 % so yay, I guess? Hip from 4.5% to 6.1%. I know my left hip is weaker in general and I’m terrible at exercising. I am doing some Tai Chi regularly and swam laps a few times a week during the summer but have to figure out what to do now. I have had PT in many parts of my body and have lots of exercises I can do. I’ve been concentrating on dealing with my neck arthritis over the last number of months so likely the back strengthening work helped my spine.
My mom had a hip replacement in her early 80’s and had lots of falls during the next several years. Like me, she had arthritis in areas like fingers; I also have it in feet and neck.
I’m pretty sure my doctor will again suggest considering biphosphonate treatment but after reading all the potential issues, I’m leery. I’m not crazy about increasing meds anyway.
Really I just felt like posting somewhere about all this! Not sure if there’s any particular advice that could help but it’s nice to be part of the community here.
I am currently reading the book Great Bones, by McCormick. He is a chiropractor, an athlete who was diagnosed with osteoporosis at a young age. The information he presents is fascinating, and you might find some of it helpful as you navigate your own journey.
I went last week for a bone density test in my new state. I just got my old records from my old state. It had this “The spine scan was technically limited because of focal sclerosis and osteophytes”. Anybody have any insight on what this means?
Osteophytes are bone spurs. Focal sclerosis on the bone is new to me. Here is something related to seeing it on a scan: Sclerotic Lesions of Bone | UW Radiology.
Got my test results back. No longer in the osteoporosis range - only in the osteopenia range. So glad I didn’t listen to that endocrinologist and I never took drugs!
I found this on a website for an imaging center. I had not heard this, and I think it’s important information:
To ensure optimal scan accuracy, you should maintain adequate hydration prior to undergoing a DXA scan. The scanner’s calibration assumes a standard hydration level, deviations from which can lead to erroneous interpretations. For instance, a hyper-hydrated state may result in an overestimation of bone density, while dehydration typically leads to underestimation.
To serve your patients effectively, it’s crucial to advise them about maintaining proper hydration before a bone density scan. This simple preparatory step can significantly enhance diagnostic accuracy, enabling more precise assessments of osteoporosis and other conditions affecting bone health.
Holy cow. That’s new information to me, and I thought I was well-informed.