My understanding is that hospitals are reimbursed the same whether an admitted patient occupies a room on the floor or occupies a stretcher in the hallway of the emergency department. As a result, there is no financial incentive to move the “boarder” into a room. In fact, the financial incentive is to keep the hospital census above capacity at all times. It’s like a restaurant serving 100 customers when it has a dining room that can only accommodate 80.
However, if all of the hospitals are overcapacity and stopped boarding from occurring, who would step up to take care of all of the patients who would be turned away?
My son was a “boarder” in a rural ER (not Portland) for 11 days, because there was not an available psych bed anywhere in the state. The ER staff were nice people, but they weren’t equipped to deal with him. Without going into details, it was NOT a good situation and he actually got injured. ![]()
This is a very simple problem to identify. The solution is probably very difficult to implement.
My inlaws’ suburban county has a single ER after two hospitals were sold and closed. The night I was admitted (long scary story) security guards were in the parking lot telling people to be aware that there was a 4 hr wait for triage, unless it was immediately life-threatening. Urgent Care ambulances were taking people 40 minutes away. I spent 75% of the time on a gurney in the crash room where they kept extra equipment.
It’s crazy out there, for staffand patients. Nothing good can come of ignoring the problem.
There need to be psychiatric intake centers. A law in Maine to create several around the state failed. ![]()
A common theme is that many healthcare facilities closed down in the past 2 decades.
There are so many medical needs that are not adequately met, yet they are saddling medical centers with helping the chronically homeless and other huge societal problems.
We need to reopen our public psych hospitals! Many noncompliant psych patients are frequent flyers who cycle in and out of the hospital via the ED. They need 1:1 nursing care, occupy ED rooms for days while they wait for a psych bed to open up. If they could be redirected to a psych hospital, they’d get prompt appropriate care, and the gridlock in the general EDs would be eased.
There is a horrible shortage of psych beds. The parents’ group I am working with in Maine did a survey. There are about 430 staffed psych beds in the whole state, and we are about #19 in the country for beds based on population.
Forensic patients (those in the criminal justice system) get priority, so people like my son who have never gotten in trouble languish longer in ERs.
My 97 yr old uncle died (non-covid related) in a Sun City West, AZ ER just after Christmas this year. They told my cousins that the hospital was experiencing the worst covid outbreak they’d seen, effecting both staff and patients. It took them two weeks to send his body back to MN because they were short-staffed.
There is a saying in healthcare that you can only choose 2 of the following
- Good care
- Fast care
- Affordable care
All 3 are subjective qualities.
It took my son 10 months to finally get good care, at the state psychiatric hospital of all places. But I’m thankful he got it.
Well we are in the ER right now. Definitely the last place I’d choose to be. We are only here because nurse on phone said H needed to be here.
There’s a woman nonstop loudly crying out in pain—they said there was someone else like that who was 19 years old earlier today.
My husband was in the hospital for three days in late December due to a serious leg infection from a basal cell removal on the back of his knee. He got the procedure a couple of weeks before Christmas, and during the follow up a few days later expressed concerns that the wound wasn’t healing, got dismissed, then on Christmas Day finally called the doc and said something is very wrong. The doc called in some antibiotics for him, but two days later, I took a look at it and the whole back of his knee was swollen and bright red. I made him go to the ER immediately.
He was actually seen quickly and admitted, but was an ER boarder for the night and next day. He got moved to a room for two days while they pumped antibiotics into him continuously. At the worst point his whole leg was extremely swollen and pink up to his groin. Both he and I caught a respiratory infection the first night in the ER and I had a cough so bad, I couldn’t visit him in person for most of the last two days. We both were coughing for at least a month.
All that being said, I think he was cared for well at the hospital (can’t say that about his dermatologist). We live in a small city near a college town so that probably helped; enough staff to deal with the college students but not a big enough population to overwhelm the two area hospitals. He was given imaging to check for clots and other concerns and they seemed to work hard to identify the type of infection to use the appropriate meds. They took blood samples frequently to monitor his white cell count. I’m thankful he received the good care because things could have gone downhill quickly.
H is getting good care—some testing and imaging. It’s less crowded than it’s been prior times when we have been here with my folks. We are currently waiting for a CT with contrast, I believe.
Phew—home from ER. All tests and imaging were OK. H is tired and will rest from a very long day. We had excellent care—PA, nurses and other staff.
My ER tale(s) was/were in 2017. I had been scheduled for knee replacement surgery in December 2016, when my daughter was coming home from college for holiday break. But the pre-op bloodwork showed elevated liver enzymes and surgery was postponed. After an encounter with an incompetent GI who insisted that I had fatty liver syndrome, I wound up in the care of the transplant team at the hospital where my late brother had a liver transplant a decade before. After a diagnostic endoscopy, I developed an uncommon side effect, pancreatitis. When I called the doctor to describe my symptoms, he advised me not to go to his hospital’s ER, where I would wind up in the hall on a stretcher for days during treatment. So I used this new-fangled car service, Uber, to go to a new free-standing ER in Brooklyn that I had heard about. They took good care of me and then offered me a bed in a hospital elsewhere in Brooklyn that their network had just absorbed. There I was treated (very!) well, and during my hospitalization, a friend brought me my laptop to submit my applications for MSW programs that were due that week. I was eventually diagnosed with a gall bladder overflowing with stones.
When I eventually had the surgery (no bellybutton surgery for me–my surgeon had to cut me open) I spent three days in the recovery room for lack of a bed, but that’s another story.
I finally had my knee surgery on 5/31.
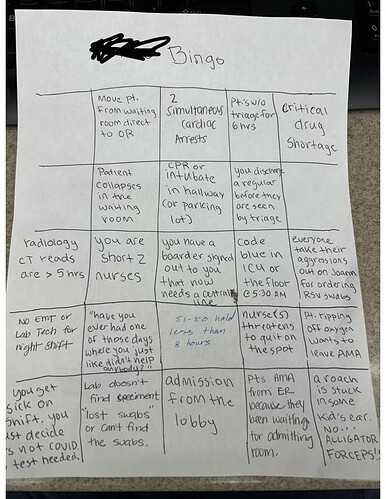
This is a bingo card my daughter made for ER staff at one of the low resource hospitals she works at These are all actual events that happened over the period of consecutive 3 nights of the same week.
Now every time the ER staff can bingo 5 events to form a row, she buys take out meals for the entire ER Dept. Take out happens almost every night.
(NOTE: the overnight shift starts at either 8pm or 10pm and ends at 6am. A code blue at 5:30am means the night shift physician isn’t going home for quite some time–often a couple of hours-- after their shift is over.
There’s only 1 physician on duty during night shift and since they are the only one trained on intubation and ACLS, that physician not only manages the ER, but also runs all code blues for the ICU and all patients floors at night.)
P.S. The night she first wrote this up, she had a patient call 911 FROM THE WAITING ROOM THREE TIMES to complain about the wait times.
Not an ER story but a recommendation: do Not use an urgent care on a holiday weekend. Completely staffed with incompetent people.